| | Circumcision and Urinary Tract Infection
Urinary Tract Infections (UTIs) are rare, and mainly occur in the first year of life. They are several times commoner in girls than boys (but of course surgery is, rightly, never considered for girls).
They are painful, and women's experience of them is a powerful inducement to have sons circumcised, if they imagine that this will protect them. In fact, a significant proportion of boys contract UTIs even though they are circumcised. A study in Israel found they mainly occured in girls at four months, but in boys soon after they were circumcised.... Now an Australian study and another from Israel suggest circumcision may cause urinary problems.
|
Jezebel, May 19, 2009
Bubble baths
One significant cause of chronic UTIs in girls, that has never been acknowledged in boys, is bubble baths, especially low-cost brands such as "Mr Bubble". In 1987, the FDA required that all children's bubble bath products carry a warning label about the risk of irritation to the skin and urinary tract from prolonged exposure. In March 2009, Mr. Bubble introduced a new "pediatrician approved" formula. |
The supposed correlation between intactness and UTIs was only discovered in 1982, long after the custom of circumcision was well-established in the US. (Yet today it is commonly presented as the first reason, illustrating how circumcision is a "solution" looking for a problem - constantly looking, as each new problem is disposed of.)
Ironically, all the 1982 paper did was quite casually note that "95% of the [male] infants [with UTI] were uncircumcised." without mentioning that virtually no babies born at that hospital (Parkland in Dallas, Texas) were circumcised. The paper went on: "All infants responded promptly to antimicrobial therapy."
Dr Thomas Wiswell |
It is Dr Thomas Wiswell who has made it his life's work to establish the UTI-intact penis connection, and he is also a keen circumcisor. His many papers present statistics involving huge samples, tens of thousands of babies (which may convince those who mistakenly think large numbers guarantee accuracy).
|
Pediatrics. 1989 Jun;83(6):1011-5.
Risks from circumcision during the first month of life compared with those for uncircumcised boys.
Wiswell TE, Geschke DW.
Abstract
The records of 136,086 boys born in US Army hospitals from 1980 to 1985 were reviewed for indexed complications related to circumcision status during the first month of life. For 100,157 circumcised boys, there were 193 complications (0.19%). These included 62 local infections, eight cases of bacteremia, 83 incidences of hemorrhage (31 requiring ligature and three requiring transfusion), 25 instances of surgical trauma, and 20 urinary tract infections. There were no deaths or reported losses of the glans or entire penis. By contrast, the complications in the 35,929 uncircumcised infants were all related to urinary tract infections. Of the 88 boys with such infections (0.24%), 32 had concomitant bacteremia, three had meningitis, two had renal failure, and two died. The frequencies of urinary tract infection (P less than .0001) and bacteremia (P less than .0002) were significantly higher in the uncircumcised boys. [It goes without saying that the frequencies of local infections, haemorrhage and surgical trauma {how serious?} were infinitely higher in the circumcised boys.] Serious complications from routine prepuce removal are rare and relatively minor. Circumcision may be beneficial in reducing the occurrence of urinary tract infections and their associated sequelae.
20 out of of 100,157 (0.02%) circumcised boys got UTIs, compared with 88 out of 35,929 (0.244%) intact boys. If circumcising the 35,929 boys would have reduced the incidence from 0.244% to 0.02% (7 boys), the Number Needed to Treat is 35,929/(88-7) = 444 circumcisions to prevent one UTI.
|
However, all the babies were born in military hospitals, where circumcision is very much the norm. It is very likely that the intact babies had their foreskins forcibly retracted. It is also likely that a major reason for the babies to be left intact was that they were born prematurly, put in intensive care and catheterised for that reason: the catheterisation, not their intactness, caused their UTIs. There are also issues around the method of determining UTI infection. Some methods of collecting urine samples risk contamination. There is a more detailed rebuttal of Wiswell on the CIRP website.
The study evaluated charts of boys born at Army hospitals worldwide and looked at those who had urine cultures and whether they were circuncised or not. Wiswell, an Army neonatologist, decided that circumcised boys had fewer UTIs based on the greater number of positive cultures. In fact, the only variable was whether the boys were catheterised, since the circumcised boys' urine was obtained by clean catch bags, while the intact boys' urine was from catheterisation, thus growing whatever bacteria were hiding under the foreskin or on the skin of the glans itself - in other
words, cultures were positive for harmless bacteria which were not causing
infection, but were simply present, as they are on all of us. The cultures
were irrelevant, but this started the whole claim that circumcision prevents UTI.
|
One commonly quoted figure is that UTIs are ten times as common in intact boys (1.1%) as circumcised boys (0.1%). This means that circumcision can offer an absolute reduction of 1% at best.
Combining the rarity of UTIs, with the only partial prevention attributable to circumcision, To et al calculated that it would take 195 circumcisions to prevent one UTI:
This figure is conservative. One factor that might make it even higher is that doctors unfamiliar with the intact penis are inclined to forcibly retract the foreskin, and this may open the way to infection.
A 2007 paper is being quoted as supporting the claim that circumcision protects against UTIs, using absurdly shonky statistics. The circumcision status of only about half of the boys with UTIs - 36 boys, a tiny fraction of the total - is known, but that is used as if it proved something.
Another confounding factor is that hospitalisiation was taken as the defining degree of seriousness of UTIs: but babies with UTIs are often hospitalised in order to be circumcised, so of course more intact babies appear in the statistics.
The main factor correlating with UTIs in infants is urinary tract abnormalities. Breast-feeding is reported to reduce UTIs' incidence (because the close contact with the mother colonises the baby's body with her benign bacteria in preference to those that cause UTIs).
UTIs are readily treated with antibiotics.
|
Does circumcision cause disease?
Prevalence of urinary symptoms in urban Australian men aged 40-69
J Epidemiol Biostat 2001;6(2):211-8 (ISSN: 1359-5229)
McCredie M; Staples M; Johnson W; English DR; Giles GG
Department of Preventive and Social Medicine, Dunedin Medical School, University of Otago, New Zealand.
BACKGROUND: This study was devised to determine the prevalence of
urinary symptoms among men living in the Australian cities of
Melbourne, Sydney or Perth, and to identify factors associated with
the presence of moderate-to-severe urinary symptoms.
METHODS: The study comprised a population-based sample of 1,216 men, aged
40-69 years, whose names were obtained through electoral rolls and who
participated as controls in a case-control study of risk factors for
prostate cancer. As part of a structured face-to-face interview, the men
completed the International Prostate Symptom Score (IPSS). Men with
moderate (IPSS = 8-19) or severe (IPSS > or = 20) urinary symptoms were
compared with those with mild or no symptoms (IPSS < 8) using
unconditional logistic regression.
RESULTS: The age-specific prevalence of moderate-to-severe urinary
symptoms (IPSS > or = 8) in men aged 40-49, 50-59, 60-69 years was
16%, 23% and 28%, respectively. Compared with men with no or mild
urinary symptoms (IPSS < 8), men with moderate-to-severe symptoms
were more likely to report not currently living as married
[odds ratio (OR) = 1.5; 95% confidence interval (CI) 1.1-2.0] and
being circumcised (OR = 1.5; 95% Cl 1.2-2.0). The increased
likelihood associated with drinking an average of > 60g per day
of alcohol in the 2 years before interview was of marginal
statistical significance (OR = 1.6; 1.0-2.6). There were no
significant differences between men with IPSS > or = 8 and those
with IPSS < 8 with respect to body mass index, education level,
having had a vasectomy, or cigarette smoking.
CONCLUSION: Among Australian men, being circumcised, or not currently
living as married, were associated with increased prevalence of urinary
symptoms.
|
More avoiding of the obvious - circumcision causes UTIs
|
A[rchives of]Diseases of ]C[hildren] Online
September, 2008
Is ritual circumcision a risk factor for neonatal urinary tract infections?
Dario Prais, Rachel Shoov-Furman and Jacob Amir
Schneider Children's Medical Center of Israel, Israel
Objective: Although circumcision is commonly believed to protect against urinary tract infection (UTI), it is not unusual in neonates in Israel, where almost all male infants are circumcised. The aim of the study was to evaluate the burden of neonatal UTI in Israel and its relationship to circumcision.
Design: Medical records of neonates (?T2 months old) hospitalized with UTI were reviewed and demographic and clinical data were collected. The second part of the study consisting of a telephone survey to assess timing and details concerning the circumcision, included two groups: the study group consisting of parents of male infants, aged 8-30 days, hospitalized with UTI and a control group consisting of healthy neonates.
Results: 162 neonates (108 males, 54 females) were hospitalized with UTI. Mean age at admission was significantly lower in males (27.5 vs 37.7 days, p=0.0002). The incidence of UTI in males peaked at 2-4 weeks of age, i.e. the period immediately following circumcision. In females, the incidence tended to rise with age. Accordingly, male predominance disappeared at 7 weeks and the male-to-female ratio reversed. In the second part of the study, 111 males (?T1 month old) were included: 48 post-UTI and 63 as a control group. While evaluating the impact of circumcision technique, we found that UTI occurred in 6 of the 24 infants circumcised by a physician (25%), and in 42 of the 87 infants (48%) circumcised by a religious authority; the calculated odds ratio for contracting UTI was 2.8 (95% CI: 1-9.4).
Conclusions: There was a higher preponderance of UTI among male neonates. Its incidence peaked during the early post-circumcision period, as opposed to the age-related rise in females. UTI seems to occur more frequently after traditional circumcision than after physician performed circumcision. We speculate that changes in the hemostasis technique or shortening the duration of the shaft wrapping might decrease the rate of infection after Jewish ritual circumcision.
[Conclusion: Not circumcising would decrease the rate of Unrinary Tract Infection.] |
Professor Brian Morris is fond of shroud-waving over the importance of circumcision where there are urinary tract abnormalities leading to vesico-ureteric reflux (VUR - urine backing up the ureters from the bladder into the kidneys). This study shows it makes no difference.
|
BJU Int. 2004 Sep;94(4):627-9.
Effect of circumcision on urinary tract infection after successful antireflux surgery.
Kwak C, Oh SJ, Lee A, Choi H.
Abstract
OBJECTIVE:
To evaluate whether circumcision during antireflux surgery can reduce the incidence of urinary tract infection (UTI) after successful ureteric reimplantation in patients with primary vesico-ureteric reflux (VUR).
PATIENTS AND METHODS:
Children who had undergone antireflux surgery for primary VUR were divided into group 1 (27, circumcised at the time of antireflux surgery at the parents' request) and group 2 (50, those not circumcised). All antireflux operations were by the Cohen method. Regular urine samples were cultured to detect UTI, which was defined as a single species with >10(5) colony-forming units/mL in a midstream voided specimen. Numbers of UTI episodes before and after surgery were compared between the groups, with (99m)Tc-dimercaptosuccinic acid (DMSA) renal scans also taken in all patients. Each scan was blindly reviewed in terms of the size, number and zonal location of cortical defects, based on morphology. Interval changes were categorised as improved, no change, progressed, and new scar formation, and compared between the groups. Prophylactic antibiotics were maintained until the follow-up studies at 4-6 months after surgery.
RESULTS:
There was no significant difference between the groups in age at the time of operation (mean 42.4 vs 47.4 months), the age at the first documented UTI (mean 26.5 vs 29.3 months), reflux grade, or number of UTI episodes and renal parenchymal scarring on DMSA before surgery. There was no significant difference between the groups in the number of UTI episodes at a mean (range) follow-up of 151.3 (114-207) months after antireflux surgery. Also there was no significant morphological change on follow-up renal scans and no difference between the groups.
CONCLUSION:<.br>These findings suggest that circumcision during antireflux surgery has no effect on the incidence of postoperative UTI.
|
Back to the Intactivism index page
The first reference is by GM Ginsberg and GH McCracken, "Urinary tract infections in young children" Pediatrics 1982; 69:409-12, according to "Neonatal Male Circumcision", a policy statement by a working party of the Australian College of Paediatrics, August 1995.
The 2007 study is P.H.Conway, A. Cnaan, T. Zaoutis, B.V. Henry, R.W. Grundmeier, R. Keren, "Recurrent Urinary Tract Infections in Children, Risk Factors and Association With Prophylactic Antimicrobials," JAMA, July 11, 2007, Vol 298, No. 2
"From a network of 27 primary care pediatric practices
in urban, suburban, and semirural areas spanning 3 states, a cohort
of children aged 6 years or younger who were diagnosed with first UTI
between July 1, 2001, and May 31, 2006, was assembled."
("States" implies the study was entirely US-based. The doctors'
affiliations (Philadelphia and Cincinatti) suggest eastern states.)
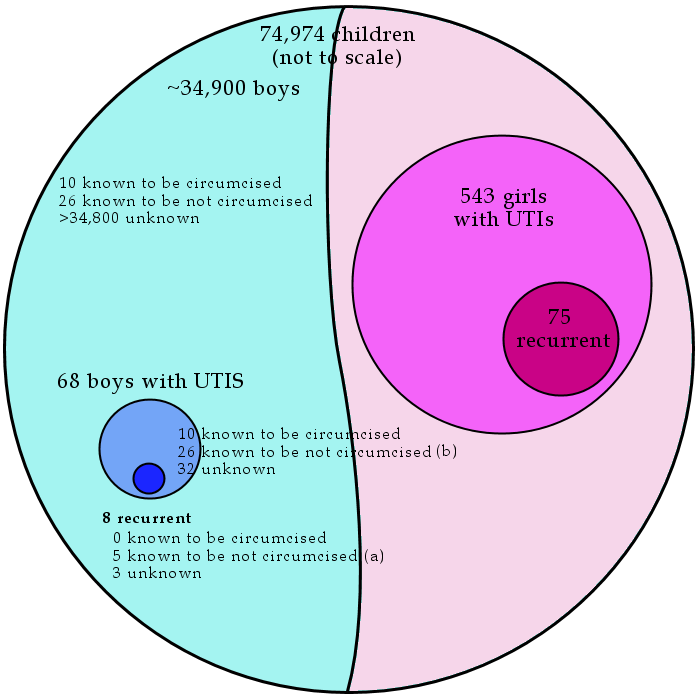
| First UTI (n = 611) | Recurrent UTI (n = 83)
|
Sex | | |
Male | 68 (11.1) | 8 (9.6) |
Female | 543 (88.9) | 75 (90.4) |
That's to say EIGHT times as many females got a first UTI as males and NINE
times as many got a recurrent UTI (but the difference between first
and recurrent UTIs is not significant: femaleness is not associated
with recurrence as such. It's probably safe to assume that the sex ratio of the 74,974-strong cohort was about 50:50, but this is not specified.
The total information about circumcision is:
"Of the 68 male children [with any UTI], there was no documented
circumcision status for 32 (47%). Twenty-six (38%) were uncircumcised and
10 (15%) were circumcised."
That is, they had no circumcision data for nearly half of those with a first UTI. This
throws the data about the other half into meaninglessness, right there.
There is also no data for the ~34,900 boys WITHOUT a first UTI,
so those percentages tell us nothing. Suppose, for a ridiculous example, that of the 35,000 males only those 10 were circumcised, then the UTI rate among circumcised males was 10/10 or 100% and among the intact only 26/34,990 or 0.074%, and a case could be made that circumcision causes UTIs and/or that intactness protects against them.
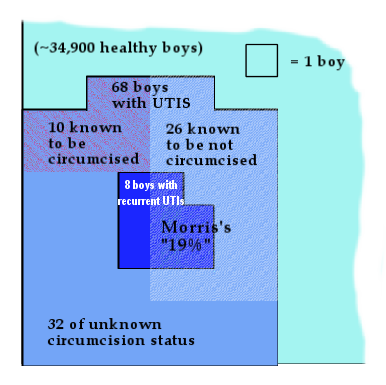
And later "Among male children in whom circumcision status was known, 5 of 26
(19%) uncircumcised vs 0 of 10 circumcised children had a recurrent
UTI (P=.13)."
(Emphasis added. P=.13 means no statistical significance.)
Without any information about the status of the whole sample, this is also
meaningless. Taking a p value, or a percentage, for a sample of 36
children is nonsense. Common sense tells you that these figures are too
small to show anything. Three more circumcised boys with recurrent UTIs (out
of ~35,000, or even out of the 32 whose circumcision status was unknown) would be 23%, overturning any claim.
To print percentages of circumcised and intact with first and recurrent UTIs in the form Conway et al. did was misleading and irresponsible.
It is also quite likely that "lack of circumcision" was more likely to be noted when a boy had a UTI than when he didn't, because of the previous work of Wiswell et al. in claiming there is a link.
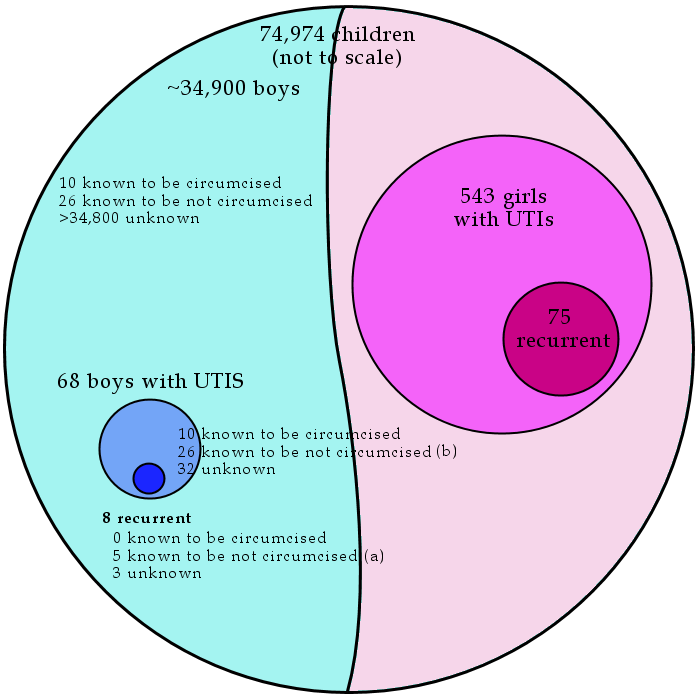
Yet Prof Brian Morris goes one step further. He has expressed this figure as “Recurrent UTIs occur in 19% of uncircumcised boys, but in none of the circumcised.”
Morris, B, Why Circumcision is a biomedical imperative for the 21st Century, BioEssays 29:11, 1151,
(Conway divided (a) by (b) in the diagram above. Morris has omitted the phrase "among male children [with any UTI] in whom circumcision status is known") Here is a closeup, to scale.
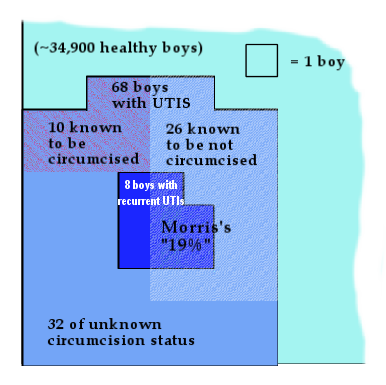
It should be clear that "19%" is a perfectly nonsensical figure.
A statistician comments:
It is not possible to evaluate whether a treatment is worthwhile
based on its Relative Risk Reduction. While a 90% reduction may
sound impressive, 90% of a tiny amount is an even tinier amount.
The Number Needed to Treat (NNT) is a much better indicator, because it makes it possible
to compare the cost of the treatment with the benefit of the
treatment.
The lower the incidence of a condition, the higher the NNT
required to prevent that condition. Because the incidence of UTI
is low, the NNT will be high irrespective of the relative risk
reduction of the treatment. Even when the relative risk reduction
is 90% the NNT is very high. The lower the relative risk
reduction, the higher the NNT (and when the relative risk
reduction is zero, even an infinite number of treatments will not
prevent a UTI).
Even though we are not given either
- the circumcision status of 32 of the 68 boys with a UTI,
or
- among the young males in the general
population to which the subjects belonged
we can calculate NNTs for various values of these
variables.
Of the 68 boys, we know that 26 were intact and 10 were circumcised,
so the total number of intact boys must be between 26 and 58. If
the circumcision statuses of an intact boy and a circumcised boy
were equally likely to have been noted, then 49 of the 68 boys with
a UTI were intact. However, where the circumcision rate is very high, it
is plausible that intact status would be considered more noteworthy than
circumcised status and thus more likely to have been noted, in which case
the intact:circumcised ratio among the 68 boys with UTIs would be lower
than the 26:10 ratio among the 36 boys whose statuses were noted.
It seems likely that the children in the study came from Ohio,
Pennsylvania and one other (possibly adjoining) state in which the
circumcision rates are very high.
A number of US studies have observed that UTI incidence among
circumcised boys was lower than that among intact boys. They have
failed to establish whether that is because circumcision reduced the incidence, or
because improper care of the intact penis in the US elevates the
incidence in intact boys (or both, or neither). Whatever the cause,
conventional wisdom has it that the incidence is about 90% lower in
circumcised boys.
Based on the data in the Conway study, it can be calculated that
- if circumcision reduces UTI incidence by 90%, and
- if the circumcision rate of young boys in the general population to which the study subjects belonged is in the range 78% to 87.5%,
then
- it probably requires between 133 and 186 circumcisions to
prevent a single UTI (almost always successfully treatable with
antibiotics) and
- it requires between 600 and
1,577 circumcisions to prevent a recurrent UTI.
It is possible that a large number of UTIs in intact boys in the US
are caused by improper care of the intact penis, i.e., that the
difference, if any, between the UTI incidence in intact boys and
circumcised boys would be much smaller than has been observed in US
studies if physicians and parents knew how to care for the intact
penis. If we assume that 50% of the UTIs
observed in intact males in the study were caused by improper care, and, if circumcision reduces UTI incidence by 80%, we can calculate that
- it probably requires somewhere between 300 and 417 circumcisions to
prevent a single UTI and
- it requires between 1,200 and 3,548
circumcisions to prevent a recurrent UTI.
If this is the case, and if one costs a circumcision at $300 (and
ignores the cost of re-circumcisions, treatment of complications and
any consideration of long-term damage), it costs
- of the order of
$100,000 to prevent a single UTI (which can be treated by a ~$20 course of
antibiotics), and
- $300,000 to $1,000,000 to prevent a recurrent
UTI.
The UTI incidence among young girls in the study was 1.48%, while
the highest credible UTI incidence among intact young boys was
0.83% -- i.e., the rate anong girls was at least 78% higher than
the rate among intact boys -- hardly a comparison upon which to
base advocating prophylactic surgery on boys.
|
| |